Sepsis can affect anyone. Its consequences will be understood by Brno scientists thanks to a grant of 6,9 euros

Jan Frič and Marcela Hortová-Kohoutková are presenting the BEATsep project.
The issue of the consequences of sepsis, known as post-septic syndrome, which manifests with a wide range of difficulties, will be addressed by Brno scientists for a period of five years, thanks to a grant of 6.9 million euros, which is a little over 180 million Czech crowns. The research will be coordinated in 11 clinical and research centers across 6 European countries. Among other goals, they aim to train an artificial intelligence tool to predict the development of consequences after experiencing sepsis. This will enable doctors to tailor treatment to individual patients.
Sepsis is a life-threatening. Our immune system reacts disproportionately to an infection, leading to damage to one’s own tissues and organs. Surviving sepsis can have long-term health consequences that significantly reduce the quality of life.

Sepsis annually affects up to 50 million people and accounts for one-fifth of global deaths. How is this possible when diseases like heart attack or oncological illnesses dominate the grim statistics? Sepsis most commonly affects patients when they are weakened in some way. Those at risk include patients after serious surgeries or injuries. Sepsis can also develop as a result of complicated diseases, such as pneumonia, meningitis, or urinary tract infections. In many cases, the true cause of a patient’s death is not just the disease itself but complications in the form of sepsis that developed as a result of the underlying illness.
Grant of 6.9 million euros and personalized care for everyone
The incidence of sepsis is increasing annually, for example, due to an aging population and growing bacterial resistance to antibiotics. In developed countries, mortality due to sepsis is decreasing, but survivors face consequences of various forms and severity. Brno researchers, as part of the BEATsep project, primarily aim to improve their lives.
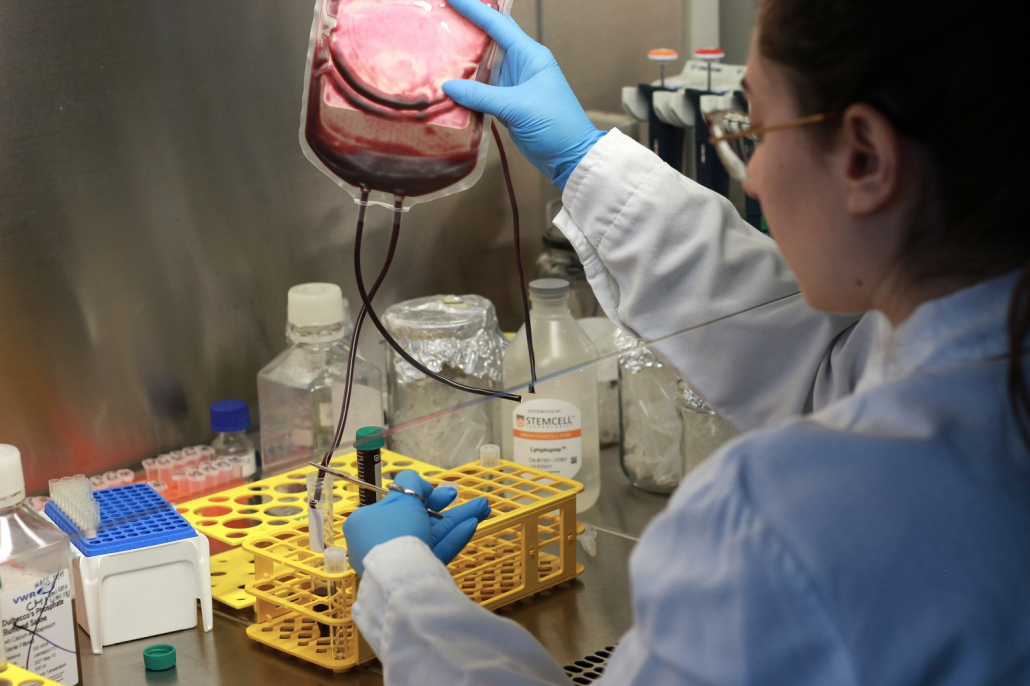
“We want to depict the condition of a patient with sepsis in detail, better understand the long-lasting changes in the body that subsequently occur, and look for combinations of suitable biomarkers that will allow us to predict how the patient’s condition will develop, and thus better tailor personalized treatment,” says Jan Frič, the head of the research team. “Our main goal is to improve the care of patients who survive sepsis but suffer from various serious consequences that complicate their lives as a result.”
The HORIZON Europe grant of 6.9 million euros was successfully obtained by the team of Cellular and Molecular Immunoregulation led by Dr. Jan Frič last autumn. “The success is even greater because our International Clinical Research Center (ICRC) initiated the entire project. It took two years of intensive work to assemble a consortium that will address the issue over the next five years. Eleven partners from six European countries are involved in the project, including institutions such as the hospital in Marseille and the traumatology institute in Vienna,” adds Frič.

BEATsep project coordinator Jan Frič.
People over 60 y.o. or children under 5 y.o. are most at risk of sepsis. In older individuals, the immune system is not as effective as in the younger population, while in small children, it is not fully developed. Other significant risk factors include the simultaneous occurrence of multiple diseases or chronic illnesses. This may lead to the misconception that sepsis does not affect the majority of the population. On the contrary, every infection can lead to sepsis. “It is crucial to recognize the symptoms of sepsis early,” says Martin Helán, who is involved in sepsis research not only within the BEATsep project but also encounters sepsis and septic shock frequently as a doctor in the Department of Anesthesiology and Resuscitation at the St. Anne University Hospital in Brno.

Doctor Martin Helán.
“When treating a severe infection, delayed treatment poses a rapid risk of sepsis progression, the development of shock, and the patient can be in life-threatening danger very quickly. Currently, we cannot predict which patient will develop sepsis and which will not. Sepsis treatment relies on two pillars – addressing the infection itself (through the administration of antibiotics and removing the source of infection, such as surgically) and supporting failing organs, for example, through artificial lung ventilation, circulatory support, or kidney function replacement,” he explains.
Consequences of sepsis? Chronic pain or anxiety and depression
Although in developed countries, 80 to 85% of people survive sepsis, a significant portion of them suffers from post-septic syndrome after recovery, which manifests in diverse ways. From neurological difficulties such as sleep disorders, concentration issues, or impaired mental capacity, to chronic fatigue or chronic pain, metabolic issues, and inadequate nutrient absorption, all the way to immune system disorders.

BEATsep project coordinator Marcela Hortová-Kohoutková.
“And this can significantly complicate the recovery of these patients,” says one of the coordinators of the BEATsep project, researcher Marcela Hortová-Kohoutková, who simultaneously leads a research work package within the BEATsep project assessing the burden after surviving sepsis. “Patients may also suffer from long-term immune system weakness, making them much more susceptible to further infections. Depression can also afflict them as a consequence of sepsis; in general, the range of difficulties is very diverse. The BEATsep project is truly a significant milestone. Thanks to the BEATsep project, doctors caring for these patients will have a simple tool that provides answers, ultimately allowing the improvement of care for those who have experienced sepsis,” she adds.
The International Clinical Research Center is a joint facility of the St. Anne University Hospital in Brno and the Faculty of Medicine of Masaryk University.


