STEM CELLS DISEASE MODELING
Patient heart on the dish – modeling inherited cardiomyopathy using stem cells
Mgr. Vladimír Rotrekl, Ph.D.
E-mail: vladimir.rotrekl@fnusa.cz
Key words
Disease Modelling, Pluripotent Stem Cells, Genome Stability, Cardiomyopathy, Stem Cell Metabolism.
Research focus
- The Stem Cell and Disease Modeling research team (SCDM) builds on long term experience with human pluripotent stem cells, their cultivation and their differentiation.
- The current focus of the team aims at the use of human pluripotent stem cells to model human diseases with special foccus on the role of tissue specific progenitors/stem cells on the development of the disease. We foccus on uncovering pathologies in pathways leading to change of cell fate, resulting in tissue failure. We further seek novel strategies to ameliorate the pathological effect on the progenitor/stem cell fate hange. We mostly foccus on processes involven in development of cardiomyopathy and heart failure in monogenic genetic diseases, such as Duchenne Muscular Dystrophy, Catecholinergic Polymorphic Ventricular Tachycardia and also on processes involved in pathological changes of hematpoietic differentiation in genetic diseasaes, such as Nijmegen Breakage Syndrome. Our group uses reprogrammed human patient cells, as well as human embryonic stem cells with edited genome, to create models of monogenic diseases involving cardiomyopathy and pathological hematopoiesis „on the dish“. The team also complements stem cell based modeling with the analysis of both animal models and human patient samples. The SCDM team has also developed novel technology to analyze mechanoelectrical coupling in stem cell derived patients, specifically cardiac syncytium based on atomic force microscope.
Main goals
- To determine the extent and mechanisms of heart and cardiovascular progenitors/stem cell depletion in human patients suffering cardiomyopathy with genetic background.
- To determine the effect of metabolic, signaling and DNA damage/repair changes on stem cell/progenitor cell fate determination resulting in tissue failure using patient specific/disease specific human pluripotent stem cells.
Technological equipment
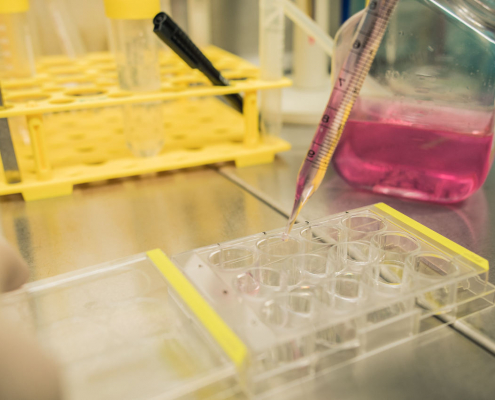
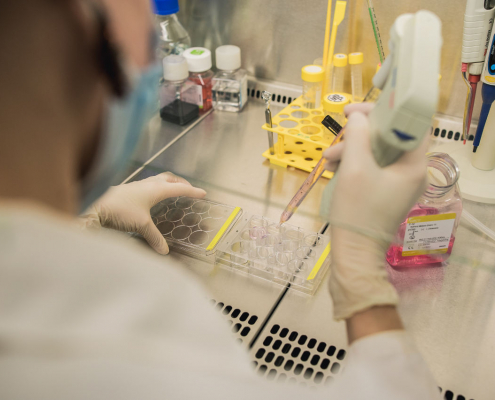
- Reprograming patient specific stem cells
- Genome editing of human embryonic stem cells
- Biosensor for drug arrhytmogenicity analysis based on coupling human pluripotent stem cell derived cardiomyocytes with atomic force microscope on microelectrode array
- Confocal microscopy
- Histological analysis
- Electrophysiological analysis of excitatory cells.